Irish pilot study sparks new hope for people with Parkinson’s disease, prolonging their ability to communicate by slowing down the progression of the disease on vocal function.
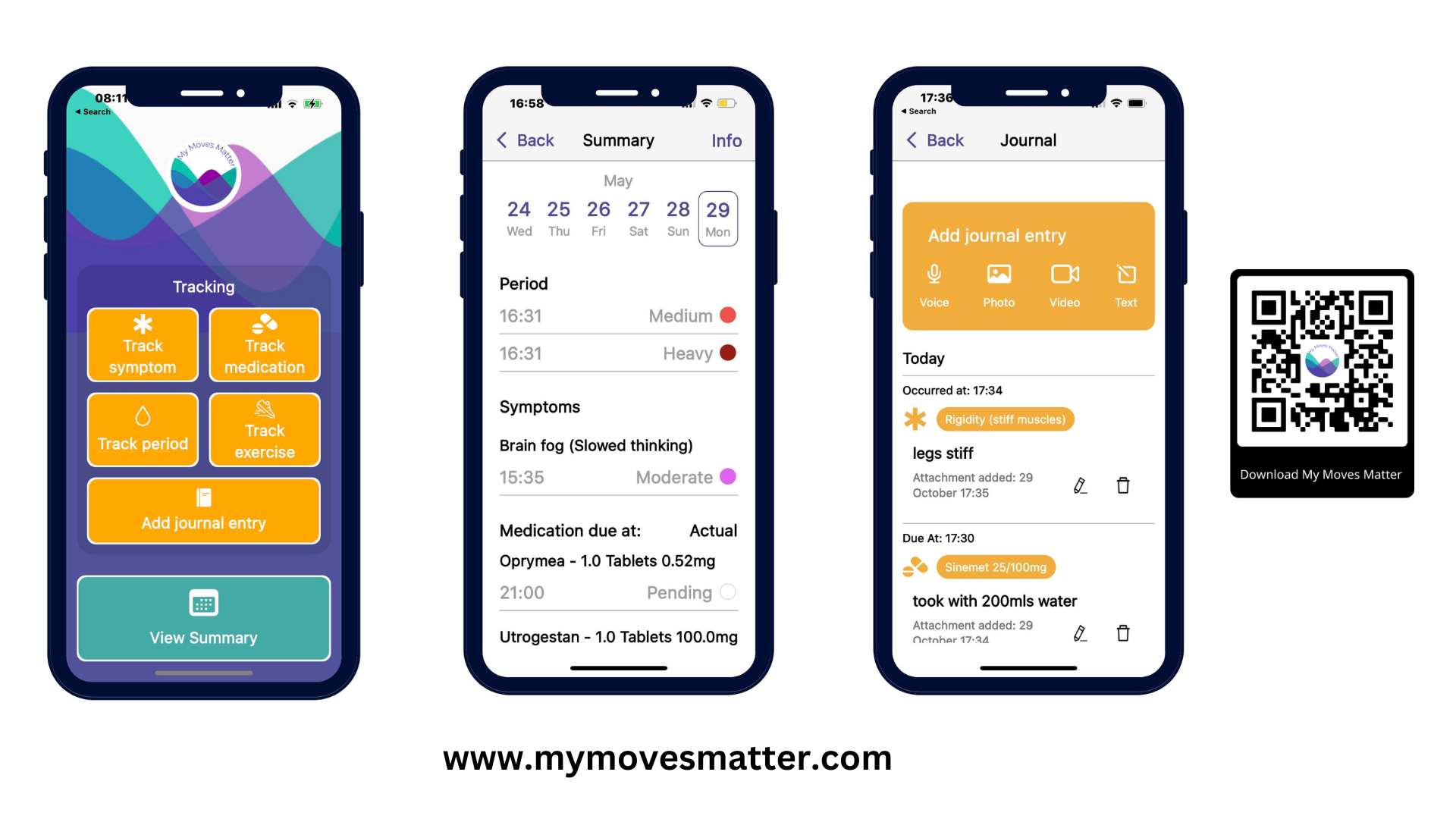
A HIHI pilot study of the Telea platform and app recorded a 10% increase in the voice of patients with Parkinsons
Pictured Telea founders Left to right Dave Calnan Co-founder and CTO Telea and Clare Meskill Telea CEO and CORU registered Speech & Language Therapist
Read the full case study here https://hih.ie/downloads/case-studies/HIHI-case-study_Telea.pdf
On World Parkinson’s Day, Telea, a Cork based start-up in University College Cork (UCC) and supported by Health Innovation Hub Ireland (HIHI) offers new hope to Parkinson’s patients with their innovative digital speech therapy technology. This will come as welcome news as in Ireland, there are almost 12,000 people living with Parkinsons.
Telea’s innovative at home therapy platform and app provides a vital connection between Speech and Language Therapists (SLTs) and patients with Parkinson’s disease allowing the SLT to monitor patient progress and treat them remotely. This platform is a gamechanger for people with Parkinson’s disease as it assists people to maintain their voice and slow down progression of the disease. The platform empowers people with Parkinson’s Disease to proactively drive intervention by increasing the quality, quantity and consistency of treatment with high dose, timely, prescribed intervention which they can do at home.
The benefits to the health system and to patients in Ireland are immeasurable. Clinically, it frees up appointments, enhances efficiency and provides remote performance analysis and biofeedback.
Parkinson’s disease (PD) is a neurodegenerative disorder that primarily affects movement. The disease gradually progresses over time and is characterised by a variety of motor and non-motor symptoms, such as tremors, changes in walking patterns, stiffness, as well as difficulties with balance and speech. At present, there is no known cure for Parkinson’s disease. Parkinson’s disease is the fastest-growing neurodegenerative disease worldwide with one in every 100 people over the age of 60 diagnosed. The journey of patients with Parkinson’s has been well documented by Michael J. Fox actor, author and Parkinson’s advocate who disclosed his diagnosis at the age of 29.
Current treatments focus primarily on managing symptoms rather than addressing the underlying cause of the disease. Speech and communication difficulties are common symptoms of Parkinson’s disease. Approximately, 90% of people with PD experience communication changes. Patients may develop weakened voice quality, can demonstrate impaired pitch variation and less clarity when pronouncing speech sounds.
When Parkinson’s disease affects a person’s ability to speak, the impact on their lives can be significant. Difficulties in communication can lead to social withdrawal and isolation. Speech therapy plays a crucial role in managing symptoms and improving communication abilities in people with Parkinson’s Disease and enhancing vocal strength.
Therefore, the marked communication improvement emerging from the results of this newly launched HIHI pilot study of the Telea platform and app now provides fresh hope for patients with the disease.
The pilot of the Telea platform was conducted with the HSE Community Health Organisation (CHO) 8 in the Midlands of Ireland working with 7 Speech and Language Therapists and 37 of their patients with Parkinson’s Disease. HIHI analysed pilot results (end-user feedback, client assessments and usage data) and prepared a final project report to disseminate outcomes with stakeholders in the Midlands and other Community Health Organisations.
Key findings were:
- the average improvement of voice was 10% across a mix of clinician-rated and patient-reported outcome measures.
- there was an 80% reduction in waiting times for SLT assessment and intervention for clients with PD. Over 80% said Telea had a positive impact on their voice.
- over 80% reported that their adherence with speech therapy exercises improved, with clients completing an average of 62 exercises per week.
- 100% of SLTs would recommend Telea to other SLTs and their clients with PD and found it easy to use. Over 85% of SLTs want to continue to use Telea.
- It was found that 60% less time was required for a typical treatment plan and 60% fewer home visits were needed.
The success of the platform and app is based on the fact that it allows SLTs prescribe exercises such as warm up, prompt to drink water, sustained vowel phonation, low-pitch and high-pitch drills, functional phrases, verbal problem solving, naming and reading aloud which can then be completed by clients through an app on their phone or tablet.
Increased efficiencies in care is a clear benefit of the product as it is designed to save time for SLTs, improve therapy for clients and reduce times for those on waiting lists for assessment and intervention. Exercises on the Telea platform focus on increasing the client’s loudness at vowel phonation of varying pitches, through personalised functional phrases and a range of cognitive tasks. SLTs can access an overview of all their clients utilising the Telea app.
Dr. Tanya Mulcahy, Director HIHI Ireland commented on the results of the pilot
‘The results of this study were very impressive, we showed that when healthcare staff (SLTs) and people with Parkinson’s used the Telea technology, waiting times were reduced, patients engaged with their exercises more than ever and there was a notable improvement in their speech. Everyone involved in this study is passionate about improving outcomes for people with Parkinson’s. Technology has the ability to enable that and we were delighted to be part of this work supporting an Irish product, Irish patients and their healthcare teams’
Claire Meskill, CEO and founder of Telea highlighted the importance of the pilot. “The value of the HIHI pilot for Telea was immeasurable as it provided an opportunity to gather invaluable feedback directly from SLTs, fostering a collaborative environment where we were able to make real-time changes and improvements based on their insights. This not only enhanced the Telea platform but also ensured it was finely tuned to meet the specific needs of management, therapists and clients in their setting.”
“The service level outcomes far exceeded our expectations and speak for themselves in terms of cost and time savings, promoting an efficient, high quality service. We are delighted to say we have secured HSE funding to continue and scale up our work with the Telea platform and to expand usage across the CHO8 region.” Ms. Aoife Carolan, Clinical Specialist SLT, Older Persons Services, CHO8
Praise from one of the Parkinson’s patients on the pilot “From day one, I loved it. I can feel the strength in my voice since I started the app. It is fantastic.”
![]()