Tuesday, 24 November 2020
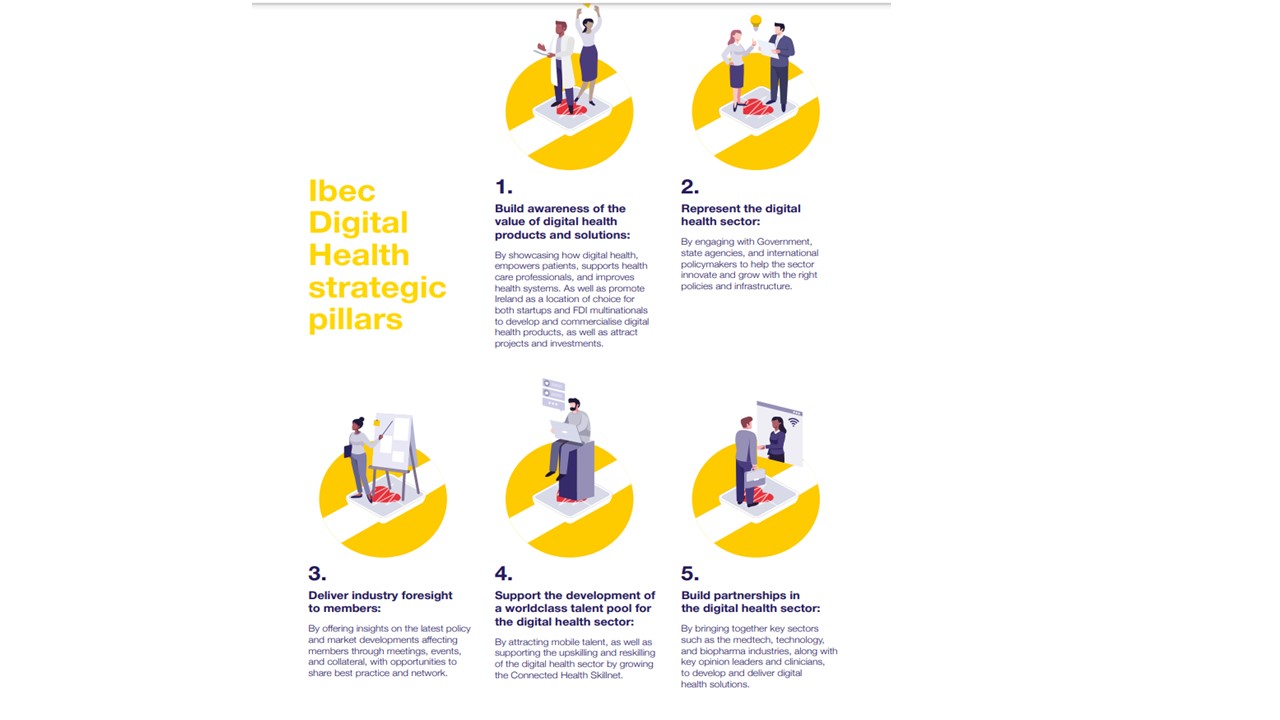
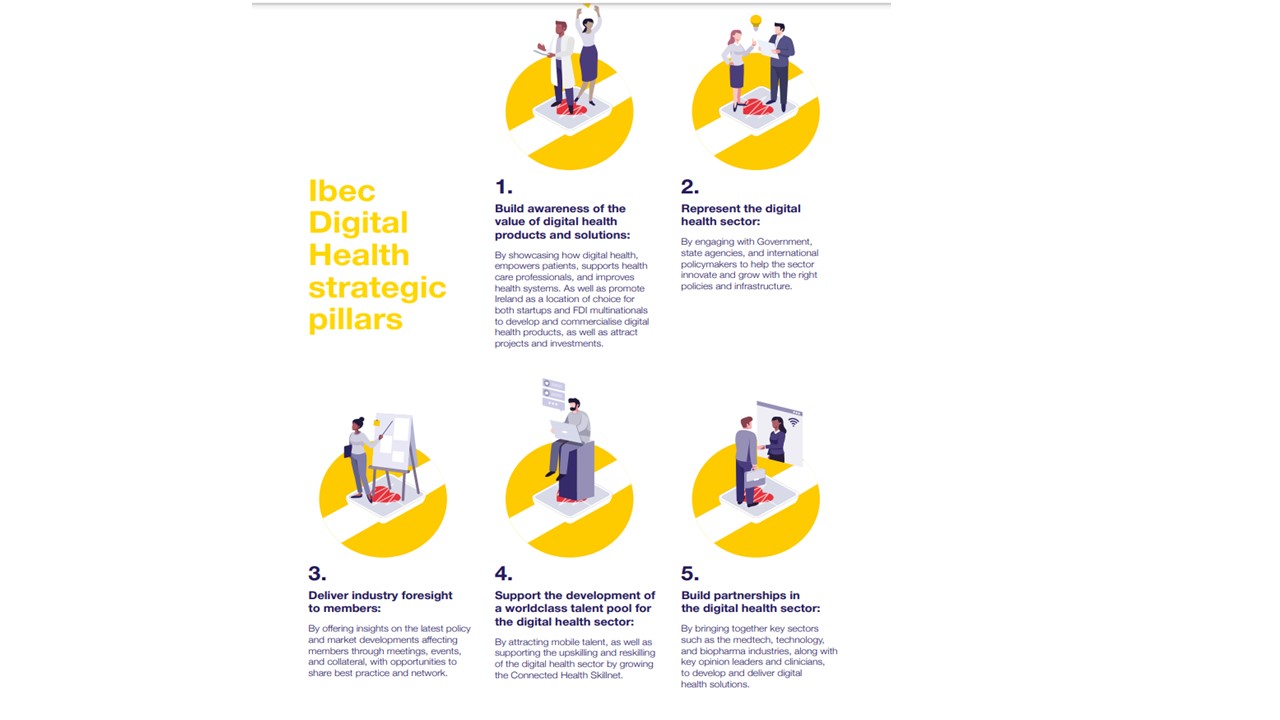
Ireland has the potential to become a leader in the development of digital health solutions, attracting international investment and growth in high-tech indigenous companies. The claim is made as part of a new campaign- Where Digital Health Thrives- launched jointly by Ibec’s Irish Medtech Association, BioPharmaChem Ireland and Technology Ireland.
Digital health is the intersection of healthcare and technology and involves the innovative use of technology to deliver better patient care. The goal is to translate the benefits that technology has brought to other industries and bring them to healthcare, resulting in improved outcomes for patients and the providers of healthcare.
Where Digital Health Thrives aims to raise understanding of the potential of digital health, and Ireland’s potential to be a hub for its growth. The campaign was launched virtually today by Jim O’Donoghue, Chair of the Ibec Digital Health Working Group and President of S3 Connected Health.
Speaking at the launch, Mr O’Donoghue said;
Digital health is driving the personalisation of medicine and healthcare, putting the patient at the centre of their treatment in an informed and supported manner. Through connected devices, remote monitoring, apps and other technologies patients are empowered to manage their health and receive care in the right setting.
Digital health is supporting health care professionals by offering insights and providing them with new ways to support and treat patients. With data from connected devices HCPs can measure outcomes, personalise healthcare interventions and better connect with patients in multiple care settings.
This campaign is about demonstrating how Digital health can lower the cost of, and increase access to, healthcare. This not only leads to improved outcomes for patients and HCPs, but for payers and providers too.
Also speaking at the launch, Sharon Higgins, Director of Member Services in Ibec said;
We wanted to capture the scale and scope of the digital health ecosystem already here in Ireland, including nearly 200 companies already delivering digital health solutions such as telehealth, data, analytics and cyber security, health information technology, connected medtech, mobile health and many more.
Ireland is the 7th most competitive economy in the world. It is a location of choice to start and grow a business. Going Global from Ireland is in our DNA. Ireland is small open economy with a global outlook. We are a location of choice for FDI investment and home to world-class start-ups. Our business model is underscored by substance and has helped us achieve a global footprint. We can apply this to digital health by delivering solutions across boundaries and borders. Ireland’s unique ecosystem with leading digital health, medtech, pharma, and tech companies can make us a global digital health powerhouse.
Ibec is uniquely placed to support cross sectoral innovation and product commercialisation. The Irish Medtech Association, Technology Ireland and BioPharmaChem Ireland came together to develop and deliver this campaign which spans a publication, ecosystem map, digital collateral and networking events. Training will be delivered in partnership with Connected Health Skillnet, which was established in Ibec in 2017 to support the drive skills development in this area.
Source: https://www.irishmedtechassoc.ie/IBEC/Press/PressPublicationsdoclib3.nsf/wvIMDANewsByTitle/ireland-aims-to-be-recognised-global-hub-for-digital-health-24-11-2020?OpenDocument